Fractures
What kinds of injuries affect bones and joints?
Fractures are broken bones. Sometimes they’re small fractures, that are barely detectable and MRI imaging needs to be used. Sometimes they’re large fractures that may require splinting or casting. Some fractures may even require surgery. At a physiotherapy clinic, there are a few roles we can play with fractures. For some of the smaller fractures, that don’t require splinting or casting, physiotherapy can help to identify and address the issues that caused it in the first place, for example with stress fractures. For the larger fractures that require periods of immobilisation, physiotherapy can help to maintain and restore muscle mass, and restore normal biomechanics (body movement) and range of motion when the fracture has healed.
What happens to the body?
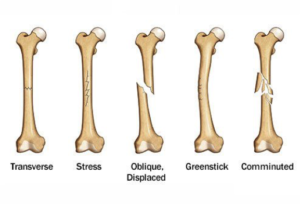
Fractures occur when the bone is exposed to more force than it is capable of withstanding. There are several classifications of fractures:
Stable Fractures – the broken ends of the bone line up, or are barely out of place. This fracture type generally includes minor stress fractures, and any type of fracture that is only a partial break, such as greenstick fractures.
Compound Fractures – this is when the skin is broken either by the bone, or by the blow that caused the fracture.
Transverse Fracture – this type of fracture runs perpendicular to the line of the bone.
Oblique Fracture – this type of fractured is angled when compared to the line of the bone.
Comminuted Fracture – this type of fracture occurs when the bone is shattered into 3 or more pieces.
What to do and what not to do?
- If the suspected fracture is in the spine, you must visit the emergency room immediately.
- Avoid painful movements unless instructed otherwise. Pain is your brains way of saying there is something wrong with a body part. Generally avoiding painful activities is a good idea. Sometimes your physiotherapist may encourage you to work through the pain, but leave that one to their discretion.
- If the suspected fracture is in the lower limb, avoid weight bearing on that limb.
- Initially, using ice can help to reduce pain. This can help to numb the area. Avoid using for prolonged periods of time as this can lead to a burning effect on the skin.
- Compression support can help during the initial phase, and during the first few weeks of your injury. This can help to reduce swelling and may help with blood flow (blood is essential for healing).
Osteoarthritis
What kinds of injuries affect bones and joints?
The most obvious one is a muscle strain or tear. The term “strain” is usually used to describe a mild, or grade 1 tear. This is a tear of less than 10% of the muscle fibres, strands of muscle tissue within the muscle belly. The term “tear” is usually used to describe something more serious, i.e. a grade 2 muscle tear, in which up to 90% of the fibres are damaged. When a muscle tears completely, that is usually referred to as a “rupture”. In this case, 90-100% of fibres have been damaged. “Avulsion” is another term used to describe complete rupture, but is normally used to describe a situation where the tendon of the muscle is torn from the bone. Muscle strains and tears usually occur as either an overstretch of the muscle, or contracting under too much load for the muscle to handle.
What happens to the body?
Muscle tears involve disruption of the fibres that shorten the muscle belly, which in turn disrupts the muscle’s ability to move you. If muscles fibres are torn, these fibres won’t be able to add to the amount of force that your muscle can produce. This will weaken the muscle, and will most likely cause pain as your try to contract your muscle. If you try to stretch the muscle, this can potentially pull on the damaged muscle fibres, which can also lead to pain and muscle guarding. At this point, you may start to notice changes in your biomechanics (body movement), which can lead to completely new issues. If you have completely ruptured a muscle, this means you will be unable to contract the muscle at all. With a complete rupture, you may notice the muscle belly ‘bunching’ at one end.
What to do and what not to do?
- Heat can be a nice way to reduce the pain associated with OA. A warm shower or bath can help to relieve the aches, and restore some movement in the joints affected. Heat packs and heat rubs can also be effective.
- Movement is a great way to improve quality of life with OA. Gentle stretches in the morning can help to get the day started, and walking has a lot of benefits for providing nutrition and healing for the joints.
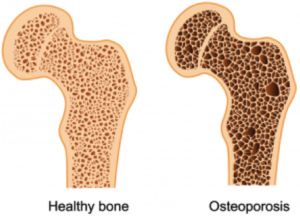
Osteoporosis
What kinds of injuries affect bones and joints?
Osteoarthritis (OA) is, in simple terms, degeneration. Although this is a normal process of aging, it can lead to pain in the joints, and therefore can lead to reduced mobility. This can lead to a whole host of other complications, so it’s extremely important that we are able to keep ourselves moving as we age. OA mostly affects the older population, but in some cases can be found in young to middle aged populations.
What happens to the body?
OA describes degeneration of the joint, and the inflammation that occurs as a result of that. It’s worth noting that the level of pain that you feel does not necessarily correspond with the level of degeneration of the joint. With this in mind, pain in the joint can be minimised through physiotherapy.
What to do and what not to do?
- Resistance training is an important way to not only slow the deterioration of the bones, but also, in some cases, to reverse the effects and strengthen the bones. Make sure you consult your clinician before beginning any exercise program.
Joint Sprains
What kinds of injuries affect bones and joints?
Ankle sprains are a very common injury, and in fact one of the most common injuries that people visit a physiotherapist to address. However, ankles are definitely not alone for sprains. Sprains are tears in the ligaments that support a joint. Other common sites for sprains are knees, shoulders, elbows and wrists.
What happens to the body?
Joint sprains describe injury to a ligament. A ligament is a piece of fibrous material that attaches usually from one bone to another, to increase the stability of a joint. Sprains can be grade one (up to 10% of fibres torn), grade two (10-90% of fibres torn), or grade three (90-100% of fibres torn). Grade three tears are also know as ruptures or avulsions.
What to do and what not to do?
- Initially, using ice can help to reduce pain. This can help to numb the area. Avoid using for prolonged periods of time as this can lead to a burning effect on the skin.
- Compression support can help during the initial phase, and during the first few weeks of your injury. This can help to reduce swelling and may help with blood flow (blood is essential for healing).
- Elevation, like compression, should be used in the initial phase to help control swelling.
- Heat (heat packs or heat rubs) should be avoided if there is any redness or swelling. Redness and swelling are signs of inflammation, which may increase with the addition of heat.
Meniscus or Labral Tears
What kinds of injuries affect bones and joints?
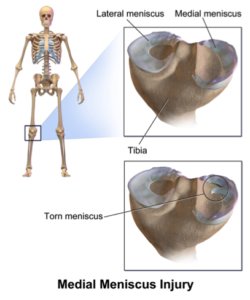
Meniscus tears refer to damage of the cartilage in the knee. These tears will usually occur from a twisting motion on the knee when the foot is planted. Labral tears are similar to meniscus tears. The most common labral injuries can be found in the hip or the shoulder.
What happens to the body?
The meniscus and the labrum are cartilaginous structures that are found within some joints to increase the congruency of the joint. When tears happen within these structures, they can be mild right through to severe. These tears can cause pain and inflammation in the joint, and restrict weight bearing and activity. In some cases, the meniscus/labrum can develop a flap, which may lead to the joint locking up. In these cases, the sufferer may lose significant range of motion.
What to do and what not to do?
- Initially, using ice can help to reduce pain. This can help to numb the area. Avoid using for prolonged periods of time as this can lead to a burning effect on the skin.
- Compression support can help during the initial phase, and during the first few weeks of your injury. This can help to reduce swelling and may help with blood flow (blood is essential for healing).
- Elevation, like compression, should be used in the initial phase to help control swelling.
- Heat (heat packs or heat rubs) should be avoided if there is any redness or swelling. Redness and swelling are signs of inflammation, which may increase with the addition of heat.
Hyper and Hypomobile Joints
What kinds of injuries affect bones and joints?
Hyper or hypomobile joints refer to joints that have increased (hyper) or decreased (hypo) range of motion. This may occur for a variety of reasons. Sometimes, this may simply be due to genetics. While we can change the mobility of joints through a variety of treatment techniques, some people will always be more or less mobile than others. Other reasons for changes may be trauma, or may be influenced by other factors such as the ones discussed above.
What happens to the body?
Unfortunately, this one is not a simple answer. To know exactly what is causing a joint to be hyper or hypomobile, a thorough history and examination must be taken. In the case of hypermobile joints, this may be due to laxity of the ligaments (possibly due to a ligament sprain), subluxation/dislocation, weakness in the stabilising muscles and a host of other possibilities. When it comes to hypomobile joints, this may be due to trauma such as broken bones, ligament sprains (which can decrease movement for a variety of reasons such as swelling and muscle guarding), degenerative changes (OA), or systemic conditions such as rheumatoid arthritis among many other things.
What to do and what not to do?
- In the case of hypermobile joints (assuming no trauma has occurred), a resistance training program may be of benefit by helping to support the joint with muscle activity. Make sure you consult your clinician before beginning any exercise program.
- In the case of hypomobile joints (assuming no trauma has occurred), a gentle stretching program may be of benefit. Make sure you consult your clinician before beginning any stretching program.
- Due to the complexity of causes that may result in hyper or hypomobile joints, it is important that you be assessed by a physiotherapist in order to determine what has led to this condition, in your case.
How do I know I suffer from a muscle injury or condition?
The first thing you may notice as a result of a bone or joint condition or injury is pain, and/or swelling. The best method for diagnosing this condition is a physical assessment, which all Musculoskeletal Physiotherapy Australia Clinicians are highly skilled at performing. During the physical assessment, your physiotherapist will assess joint range of motion and ligament integrity. If your clinician believes that you have suffered from a fracture, they can give you a referral to get an X-ray at a bulk billing clinic. If your clinician believes that you may be suffering from osteoporosis, you may also be referred for a bone density scan.