What is a Shoulder Fracture?
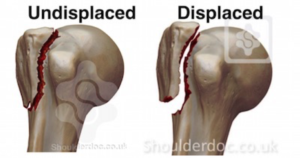
The humerus (upper arm), the scapula (shoulder blade) and the clavicle (the collarbone) all join together to make up ‘The Shoulder Complex’. A fracture, or break, to any of these bones will result in pain and loss of function to the shoulder complex. A fracture is when the continuity of the bone is broken, usually due to some sort of trauma. The level of trauma and the location of the fracture will determine how it is managed. Some fractures will be easily managed conservatively with rest and immobilisation, whereas ‘displaced fractures will require surgical intervention in order to re-position the bone parts together. X-Rays are the best way to diagnose your shoulder fracture.
Shoulder Fracture
What are the different types of shoulder fracture?
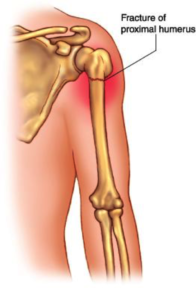
Humerus fracture
The Humerus can be fractured in multiple places, generally due to a fall or some form of trauma. Most commonly, the humerus is fractured at the ‘Neck of Humerus’ or the ‘Head of Humerus’. Depending on the type of break, surgery may be required in order to ‘reduce’ the two bone ends together.
Bony Bankart Lesion
A Bankart Lesion is a fracture to the glenoid fossa (the socket joint). It typically will occur as a result of a shoulder dislocation, when the head of the humerus makes contact with the glenoid fossa, as a result of some trauma. As there is a reduction to the bony stability provided by the glenoid, which is already limited, these lesions may contribute to ongoing shoulder stability.
Hill-sachs Lesion
Similar to a Bankart Lesion, a Hill-Sachs lesion is likely to occur as a result of a shoulder dislocation. In this case, the head of the humerus is fractured when it makes contact with the glenoid fossa as the shoulder dislocates anteriorly. These may also contribute to ongoing instability at the shoulder.
Pathological Shoulder Fractures
A Pathological Shoulder Fracture is when a disease or medical condition results in a weakness to the structure of the bone, and force or stress to the bone that otherwise would be safe, now causes a fracture. This is most commonly seen in people with osteoporosis or osteopenia, but can also rarely be seen with osteomyelitis and similar conditions. Talk to your physiotherapist about how to best prevent these fractures from occurring.
What caused my Shoulder Fracture?
Shoulder fractures are most commonly caused by falls or from direct, or indirect, trauma to the shoulder. However, in some cases it may be less obvious. Osteoporosis and osteopenia can cause a weakening of the bone that leads to a non-traumatic fracture. Conversely, applying a very high load very frequently (i.e. repetitive throwing sports) can lead to the development of stress fractures. Your physiotherapist will be able to thoroughly assess your condition and advise on the most-likely cause of your shoulder fracture.
How can you help me with my Shoulder Fracture?
Depending on the type of shoulder fracture that you have, your management will likely involve 4-12 weeks of rest and immobilisation. Your physiotherapy management will be specific to your individual presentation and based off a through examination by your physiotherapist. Your plan will typically involve light movements and therapy to gradually improve the movement at your shoulder joint, and progress to strengthening exercises as your shoulder fracture heals. Your physiotherapist will also be able address any factors that may have contributed to your shoulder fracture, such as; your bone health or shoulder instability.

What should I do to avoid aggravating my Shoulder Fracture?
- FOLLOW the advice from your Doctor about immobilizing your shoulder
- AVOID aggravating or painful activities
- DO concentrate on maintaining good posture
- KEPP your neck, elbow, hand and wrist mobile
- RECEIVE physiotherapy care to get your joints, ligaments and muscles de-loaded and moving freely with no restrictions.
Keep good care of your body and your physiotherapist will continue to monitor your condition. Once your Shoulder Fracture has resolved you will be able to resume your full activities without worrying about future flare-ups.