What is Sciatica?
Sciatica is the term used to describe the symptoms of leg pain, sometimes accompanied by tingling, numbness and/or muscle weakness. These symptoms arise from the disruption or irritation of the sciatic nerve.
Sciatic nerve pain can often vary in its intensity and frequency, however most sufferers describe a sharp, radiating pain moving up and down the back of the leg.
Sciatica, or sciatic pain is not a medical diagnosis, but rather a symptom of an underlying medical condition.

What are the symptoms of sciatica?
The sciatic nerve is the thickest nerve in your body, about as wide as your thumb, and it travels through several critical leg muscles. Irritation at any point along its path can trigger sciatica symptoms. When leg muscles tighten excessively, they can further compress the nerve, leading to worsening pain, numbness and muscle weakness.
Sciatica symptoms include:
- Constant pain shooting in only one side of the buttock or leg (sciatica pain rarely occurs in both legs)
- Pain that is worse when sitting
- Leg pain that is often described as burning, tingling, or searing (versus a dull ache)
- Weakness, numbness, or difficulty moving the leg, foot, and/or toes
- A sharp pain that may make it difficult to stand up or walk
- Pain that radiates down the leg and possibly into the foot and toes (it rarely occurs only in the foot)
Alongside the common symptoms, sciatica sufferers may also experience muscle spasms, particularly in the lower back or buttock region. Muscle weakness can develop if nerve compression is significant, making it difficult to move your foot or toes properly. If you notice changes in bladder or bowel control, seek urgent medical attention, as this may indicate a more serious underlying condition such as cauda equina syndrome.
Patients often describe pain differently: some say it feels like an intense electric shock, while others experience persistent burning or stabbing sensations. These varying sensations help physical therapists customise a treatment plan that addresses your unique experience of sciatica pain.
How does sciatica cause my pain?
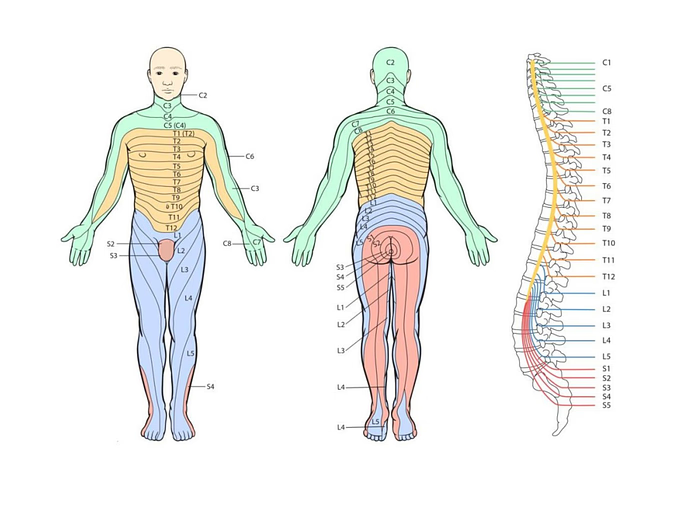
In the picture, you can see that each individual nerve root will innervate a different area of the body. These areas are called dermatomes, and while they are slightly different for each person, they can be mapped out, as seen in the diagram.
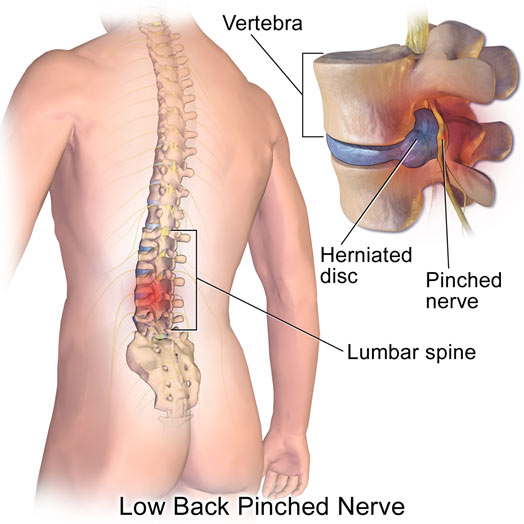
The sciatic nerve originates from nerve roots of L4 to S3 in the lumbar spine (lower back) that combine to form the Sciatic nerve, the largest single nerve in the body. Sciatica occurs when the sciatic nerve is compressed at, or near its origin. Nerve compression may occur for a number of reasons, including a herniated disc, degenerative disc disease, spondylolisthesis or spinal stenosis. In some cases, you may also develop a lack of bowel or bladder function. This is a sign of cauda equina syndrome (CES), which is a serious condition which requires immediate care.
Sciatica-like symptoms may also occur as the result of muscle tightness in the buttock region, a condition known as Piriformis Syndrome. While this is not true Sciatica, the symptoms can mimic that of true Sciatica. This is not an exhaustive list, but your physiotherapist will be able to diagnose the cause of your sciatic . The specific location of Sciatica symptoms depends on where the nerve is compressed. While sciatica can be very painful, it is rare that it results in permanent nerve damage.
In addition to nerve compression from herniated discs or spinal stenosis, muscle dysfunction can play a significant role in sciatic symptoms. When nearby muscles such as the piriformis tighten excessively, they can compress the sciatic nerve and cause muscle spasms, sharp shooting pain and difficulty walking. Manual therapy techniques used by your physical therapist can help reduce muscle spasms and tension, providing lasting pain relief and improving mobility.
Understanding the exact mechanism of your pain—whether due to disc irritation, large nerve compression or muscular causes—allows for a highly targeted treatment approach, increasing your chances of full recovery.
How do I know what is causing my Sciatic nerve pain?
A thorough assessment performed by your physiotherapist at M Physio Australia is the best way to diagnose the cause of your sciatica. They will be able to guide on any extra investigations required and on the optimal treatment plan.

What can you do to treat Acute Sciatica?
Your physical therapist at M Physio will work with you to design a complete care plan to achieve pain relief and restore function. In the early stages, the focus is often on reducing inflammation and protecting the irritated nerve through gentle movement, postural correction and pain management strategies.
Specific exercises will help strengthen weakened muscles, particularly around the core, hips and lower back, reducing pressure on the sciatic nerve. Stretching programs help relieve tightness in structures like the piriformis muscle. Manual therapy may be incorporated to release muscle spasms and improve nerve mobility.
A critical focus of your treatment is reducing muscle tension that can exacerbate nerve compression. Stretching tight muscles, improving spinal alignment and strengthening weak areas are all designed to support the healing process.
Most cases of sciatica resolve with conservative care, especially when a personalised treatment plan is followed closely. Active rehabilitation provides symptom relief while helping to ensure your sciatica resolves fully. This prevents long-term nerve irritation or recurrent flare-ups.
As your pain improves, your therapist will progressively challenge your muscles to prevent recurrence, ensuring a long-term recovery. Consistency and adherence to your exercise program are key factors in fully resolving your sciatica symptoms.
Our clinics offer sciatica treatment in Brisbane, Gold Coast or Sydney.
What should I avoid to help my Sciatica?
- Avoid smoking.
- Avoid prolonged sitting.
- Avoid sitting with slumped posture, or bending down to pick things up using a stoop lift.
- RECEIVE physiotherapy care to relieve pain and get your body performing to its optimum level.
Keep good care of your body and have regular physiotherapy treatment for sciatica to continue monitoring your condition. Once your Sciatica has resolved you will be able to resume your full activities without worrying about future flare-ups.

How Physiotherapy Management Helps Sciatica
At M Physio Australia, your sciatica care starts with a comprehensive clinical diagnosis, often including a combination of physical tests to assess nerve function, muscle strength and mobility.
Your physiotherapist may test your ability to keep your leg straight while lying down (commonly known as the straight leg raise test) to detect nerve irritation. Other physical tests help pinpoint the root cause, whether it’s a disc injury, bone spurs or muscular compression.
Based on your diagnosis, a personalised physiotherapy management plan is created, blending hands-on therapy, motor control exercises and strengthening programs to get you moving pain-free again.
Manual Therapy to Ease Sciatica Pain
Manual therapy is one of the core techniques physical therapists use to ease sciatica pain. It includes hands-on methods like joint mobilisations, soft tissue massage, trigger point release and nerve gliding techniques. These methods help reduce inflammation, alleviate muscle spasms, restore range of motion and promote healing.
By carefully targeting tight muscles and stiff joints, manual therapy improves your symptoms and addresses the underlying causes of nerve compression. It is particularly beneficial when muscle tightness or joint dysfunction is contributing to sciatic nerve irritation.
Combined with tailored exercise programs, manual therapy can provide rapid, meaningful improvements for patients struggling with severe pain.


How to Describe Pain to Your Physical Therapist
Describing your pain in detail helps the physiotherapist have your sciatica diagnosed accurately and to create an effective plan to treat sciatica.
When discussing your symptoms, try to include:
- Where the pain is located
- Whether it is sharp, burning, throbbing or stabbing
- If the pain radiates, and how far
- If pain worsens when sitting or bending
- Whether you have associated symptoms like muscle weakness or muscle spasms
- Mention any changes in bowel or bladder control, even if they seem minor.
Providing a detailed description allows your therapist to determine the most appropriate treatment techniques.
Understanding the Nervous System and Sciatica
Sciatica is a classic example of how the nervous system responds to irritation or injury. When a nerve root in the lower spine becomes compressed or inflamed — often due to a disc herniation or bone spurs — it can cause symptoms that radiate down the leg. This is known as lumbar radiculopathy.
The sciatic nerve’s role in transmitting sensory and motor signals means that when it’s affected, it can disrupt sensation, strength and even normal movement patterns.
Physiotherapy focuses on calming the nervous system’s heightened response, easing pain and restoring healthy function.


When Sciatica Becomes an Emergency
While most cases of sciatica can be managed conservatively, severe pain, sudden and profound muscle weakness, or loss of bowel or bladder function could indicate a medical emergency. If you suddenly cannot control your bladder or bowels, or if numbness spreads through your inner thighs or groin, seek immediate emergency care.
These symptoms may signal cauda equina syndrome, a rare but serious condition requiring urgent surgery to prevent permanent damage. Your physiotherapist will always screen for these red flags and ensure you get the right level of care if these symptoms arise.
Tips & Exercises for Sciatica from Our Physiotherapists
Our team strongly encourages self-management techniques to empower patients during their recovery. These include gentle home exercises, mindful movement, heat or ice application, and postural corrections (such as sitting with your knees bent and feet supported). If you are experiencing pain, do not perform exercises until you have been advised by your physiotherapist.
While very short periods of bed rest may be helpful during episodes of extreme pain, prolonged bed rest can actually delay recovery. Instead, gentle activity and guided exercises will promote healing and help you resume normal function faster.
Watch these videos for information and physical therapy exercises for sciatica.
Motor Control Exercises for Sciatica Recovery
Motor control exercises are essential in the rehabilitation of sciatica. These exercises retrain the deep muscles that stabilise your lower spine and pelvis, reducing strain on the sciatic nerve.
Poor motor control can contribute to recurring episodes of sciatic pain, especially if small muscles around the lumbar spine aren’t activating properly.
A targeted program, guided by your physiotherapist, strengthens these stabilising muscles, improves posture and supports better spinal movement, leading to long-term relief and prevention of future flare-ups.
Sciatica Treatment Sydney, Gold Coast & Brisbane
Struggling with severe sciatic nerve pain?
Book an assessment with our experienced physiotherapists today and start your journey toward lasting pain relief. Whether you’re dealing with muscle spasms, muscle weakness or worrying signs like changes in bladder or bowel function, we are here to help.